NEXT STORY
Moving to the Fox Chase Cancer Center
RELATED STORIES

NEXT STORY
Moving to the Fox Chase Cancer Center
RELATED STORIES



We found this lipoprotein and we got all excited, because that meant that our hypothesis, if you use this transfuse serum, you could find polymorphisms. Well, if a hypothesis works once, it can… you can work again. And again you have to think about, you know, hypotheses have several meanings. One of them is you make a hypothesis and you test it and you support it and you say well, that's a kind of statement of what's going on, you've described what's happening, which is true for the time being, because most hypotheses eventually get rejected, so it's not exactly truth, you know, it's the truth for the time being. But the… the… some, you know, they remain in… in altered form. But another value is that it's a… it’s a generator of experiments, it's an engine of experimentation and that's… that’s often the case.
So we had evolved a kind of very simple technique and it used very simple equipment. These studies using the transfused serum were done on agar gel, and you could make a plate on a… on a, you know, small glass plate, and you can buy this agar gel for very little money; you could have all the equipment you need with an expenditure of under $100. So… and we could use it in the field, too. We developed, you know, methods so that we could… I could take them with you, you could work in a hotel room, or a train, or things like that. So, we continued looking for more antibodies and we found several, but one that really looked interesting was one… was one that was clearly different from the lipoprotein polymorphism it first reacted with it, and it was very rare. Instead of being a kind of polymorphic distribution of the kind that we had seen in the past, this… we only… initially only found one, a small group of people who reacted with this particular antiserum. So this was an antiserum from a transfused patient from New York City and the early studies were done on serum from an Australian which was this panel, you know if you are looking for variation, then you use different populations because the prevalence or the frequency of… of the gene would vary from population to population, we knew that from what we knew about polymorphisms. So here we had, there was this antibody from a patient in New York City reacting with a... antigen that was present in an Australian. Now as far as we knew, neither of those people were — well, the transfused patient had… had some illness that required it - he had hemophilia - but it didn't seem to be related to this antibody and the… the Australian who had the antigen, was a non-hospitalized person as far as we understood it, he or she wasn't receiving, it was he actually, wasn't… wasn’t ill. Well, the question was what was it? And… all right, so what do you do? You have to get more data; you start collecting more information from which to make the next hypothesis. So we collected a lot of... we did lots of studies, you can do them very quickly, you can do hundreds of experiments, you know, in the… in the course of a week, and we learnt a lot about distributions. So this antigen was rare in the United States; we… we… I think we tested a thousand people before we found somebody in the United States normal population, but it was quite common in Australian, some Australian groups, Australian Aborigines mostly and… and we found that it was in Japan and China and Korea, because we had serum from those locations. And… okay, so we knew that it had a strange geographic distribution; you find it... it seems to be more in Asia and the Tropics, but rare in the United States.
Well then, in a way by chance, we looked at serum from people with different illnesses. As a matter of fact we looked at the serum… we looked… we looked for reactions with the antibody in people who had been transfused and we found that there was a very high prevalence in patients with leukemia, certain forms of leukemia, and that was… we found it because we had been looking at many diseases, and that was a higher prevalence. So we said well, there’s… there’s… you can make several hypotheses: one is that the - we called it Australian antigen - that Australian antigen caused leukemia, A causes B; the other possibility was that if you have leukemia, then you get the Australian antigen, so B causes A; and a third possibility is that there’s some factor, an inherited factor, that makes it likely to get both leukemia and the Australian antigen. By the way, those are not mutually exclusive, all of… you know, A can cause B, B can cause A, and C can cause A and B. In general that can… that’s a… this cause and affect business is a bit, you know, you’ve got to be careful about people who can… cause and affect, what you want to understand is process, you know, what's happening, not what starts it first, you very often can't tell anyhow. But anyway, we started testing, researching all those hypotheses at the same time, which meant more fieldwork, and more clinical work. So we decided we'd look at… we'd test the third part, which you can do pretty fast. We said we would look at people who have, who have… who are likely to get leukemia. So that includes people who’ve had radiation, the people who were within a thousand meters of Ground Zero, at Hiroshima and Nagasaki, children with Down syndrome. There‘s a strange kind of leukemia that is very common, well, much more common, in Down syndrome kids than in other children and which… from which they often recover. And there are several… several other possibilities. So we systematically went about getting blood from those populations. And so we had our hypothesis and it proved true in some places but not in others. But the most interesting one was the patients with Down syndrome. Now in those days, Down syndrome kids were kept in large institutions and just about that time, they began to close the large institutions and that happened within the next few years. But we found a 20–30 percent prevalence of Australia antigen in Down syndrome children, much lower prevalence in children with other kinds of mental retardation. But again, see, we had made this hypothesis, we didn't find it in some of the other places, but we did find it there. So, great, you know, now that again is another engine to do more experiments and we were able to study the Down syndrome patients.
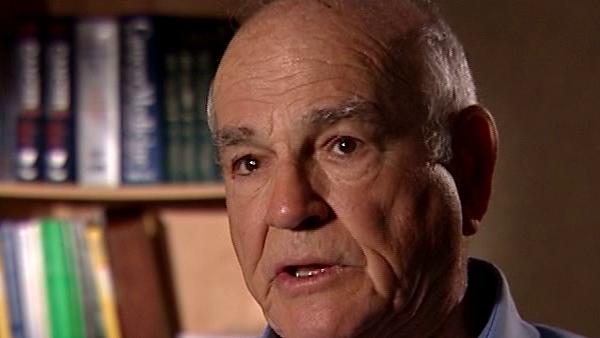
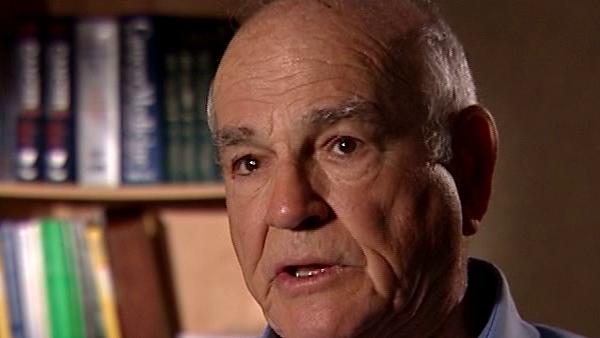
American research physician Baruch Blumberg (1925-2011) was co-recipient of the Nobel Prize in Physiology or Medicine in 1976 along with D Carleton Gajdusek for their work on the origins and spread of infectious viral diseases that led to the discovery of the hepatitis B virus. Blumberg’s work covered many areas including clinical research, epidemiology, virology, genetics and anthropology.
Title: Discovering the Australia antigen
Listeners: Rebecca Blanchard
Dr Rebecca Blanchard is Director of Clinical Pharmacology at Merck & Co., Inc. in Upper Gwynedd, Pennsylvania. Her education includes a BSc in Pharmacy from Albany College of Pharmacy and a PhD in Pharmaceutical Chemistry from the University of Utah in Salt Lake City. While at Utah, she studied in the laboratories of Dr Raymond Galinsky and Dr Michael Franklin with an emphasis on drug metabolism pathways. After receiving her PhD, Dr Blanchard completed postdoctoral studies with Dr Richard Weinshilboum at the Mayo Clinic with a focus on human pharmacogenetics. While at Mayo, she cloned the human sulfotransferase gene SULT1A1 and identified and functionally characterized common genetic polymorphisms in the SULT1A1 gene. From 1998 to 2004 Dr Blanchard was an Assistant Professor at Fox Chase Cancer Center in Philadelphia. In 2005 she joined the Clinical Pharmacology Department at Merck & Co., Inc. where her work today continues in the early and late development of several novel drugs. At Merck, she has contributed as Clinical Pharmacology Representative on CGRP, Renin, Losartan, Lurasidone and TRPV1 programs and serves as chair of the TRPV1 development team. Dr Blanchard is also Co-chair of the Neurology Pharmacogenomics Working Group at Merck. Nationally, she has served the American Society of Clinical Pharmacology and Therapeutics on the Strategic Task Force and the Board of Directors. Dr Blanchard has also served on NIH study sections, and several Foundation Scientific Advisory Boards.
Tags: Austrialia
Duration: 8 minutes, 10 seconds
Date story recorded: September 2007
Date story went live: 28 September 2009