And it was absolutely clear that there was, from what we knew already about monogenic diseases, that it was going to be complicated, but I think the, as it’s turning out and through the successes over, that had been announced in the last few weeks, there’s no question that it’s going to have enormous impacts on clinical practice. Whether, I think, and probably the cancer field has been the most impressive, I mean, where amazingly to me actually, I mean, it’s been to, possible to, apart from diagnostics obviously, to direct drugs at mutant onco genes, I mean, I would have never guessed that the chronic myeloid leukaemia story would have broken, that you could target a drug at a kinase, which was firing off, and like that, and you know, so specifically together, it turned off every ruddy kinase in the body. But, so, so I think this report that we wrote was directed at, not so much the whole thing, but at the concept of personalised medicine in the type of thing we were told by a pharmacologist at my retirement party in Oxford, that in 20 years time, every GP will have your printout, the whole of your genome printout on his desk. You go home with a headache, press a button, tell you whether you’re a two aspirin or a one aspirin man. And in fact, you wouldn’t even have to go to your GP because you can, it will all be kind of online and, and it sounds a little bit unlikely, but this was, we investigated pharmacogenetics, or pharmaco genomics, and what troubled me really, or interested me, was that when I was in Baltimore in 1960, David Price Evans on the next bench had just finished a lovely study showing that there’s no question that isoniazind metabolism was under the control very much, of one gene, depend, and that, based on the, that polymorphism, you either metabolised it rapidly or slowly. And then it turned out that if you were a slow metaboliser you’re more likely to get some of the nasty complications. That was 1960 and we, I guess, we did learn the actual molecular mechanism much later, but that has never been used in clinical practice to my knowledge. And at the same time there was the warfarin polymorphism broke, and because that’s a terribly important drug, thousands of people on it, lots of side effects, but again, that’s never been used in practice. And of course over recent years, now one has both the molecular bases for the metabolism of warfarin and varying activity due to its endorgen effect, so you’ve got two major polymorphisms, common polymorphisms in the population. A fantastic amount of information about other drugs, the pharmaceutical industry of course, one could see major practical advances, ah, advantages for them, and particularly in starting to avoid developments in areas where from a pharmaco genetic point of view was obviously looking at toxicity and so on. But, personalised medicine, so, if we took warfarin as an example, what you’d want to know is really in terms of patient effectiveness, that’s both controlling of whatever you’re trying to control, plus awful side effects. Was a pre-knowledge of their genetic make up going to be effective, and cost effective, compared with just shoving the drug in at the usual dose and very careful monitoring. And it seemed to us, at least seemed to me, I think that the others agreed, that the only way to find out was to do it in a proper population study, which is easier to kind of throw out as a suggestion than to do it. I think it’s a very difficult study. Happily the government have given one or two grants as you know, for this kind of thing, and the Liverpool school, a pharmacogenetic group, are doing just that study with warfarin. It will take them a long time. And then I think there’s another group doing a similar thing with anti-depressants. So, I think, we’ve just got to wait and see, but, so yeah, personalised medicine, I suppose it will become slightly more personalised, but I think this image that we were thrown of, and then there were, there was a very interesting thing to do, because we had public, we had meetings, the social scientists who, very skilled now at getting at the average men to meet you, the average persons to meet you, sorry, and they were very interesting actually. I didn’t, I didn’t sense concern with what people were doing in genetics so much. Their concerns were very practical. Okay, once you’ve got this information, who’s going to handle it for us? Are we going to have to rely on our GP or our pharmacist? And then of course, there are huge problems about the level of education in genetics still, in medicine, and even worse, the total decline in clinical pharmacology as a speciality, and very badly taught, so there were really quite a lot of issues came out of this, but I think to a lot of people it was terribly conservative. I think the term probably addressed at the chairman of that was a boring old fart, I heard several times, but there we are.
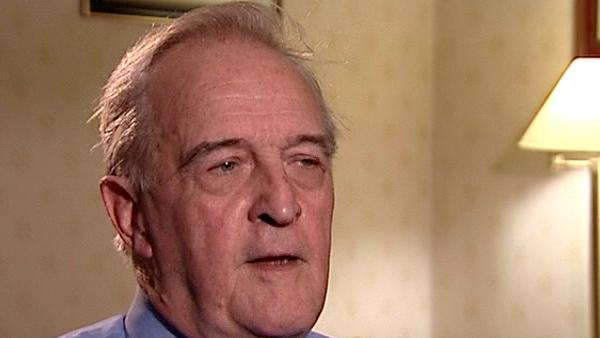
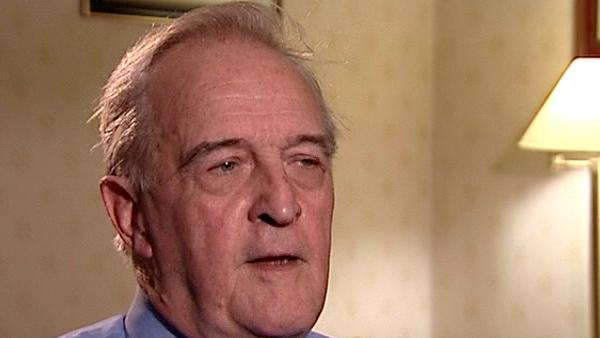
British Scientist Sir David Weatherall (1933-2018) was a world renowned expert on blood diseases, in particular thalassaemias, and used his expertise to help control and prevent these diseases in developing countries. He founded the Institute of Molecular Medicine at Oxford in 1989 and was knighted in 1987.
Title: Personalised medicine (Part 2)
Listeners:
Marcus Pembrey
Marcus Pembrey, now Emeritus, was Professor of Paediatric Genetics at the Institute of Child Health, University College London and consultant clinical geneticist at Great Ormond Street Hospital for Children London. He is a visiting Professor at the University of Bristol UK, where he was the Director of Genetics within the Avon Longitudinal Study of Parents and Children until 2006. A past president of the European Society of Human Genetics, he is also the founding Chairman of the Progress Educational Trust.
Duration:
6 minutes, 55 seconds
Date story recorded:
July 2007
Date story went live:
02 June 2008