NEXT STORY
Testing propranolol: A non-selective beta blocker
RELATED STORIES

NEXT STORY
Testing propranolol: A non-selective beta blocker
RELATED STORIES


|
Views | Duration | |
|---|---|---|---|
| 1. My journey from a mining community to a scholarship at St Andrews | 3 | 720 | 06:00 |
| 2. Highlights of the St Andrews and Dundee Medical Schools | 318 | 04:10 | |
| 3. A year in the physiology department at St Andrews | 1 | 263 | 02:57 |
| 4. Working in Singapore | 288 | 04:01 | |
| 5. Setting up a physiology department at Glasgow Veterinary College | 218 | 02:42 | |
| 6. Developing the idea of a beta receptor antagonist | 2 | 424 | 06:53 |
| 7. Working in the dream world of Imperial Chemical Industries | 308 | 03:41 | |
| 8. The accident that led to beta blockers | 3 | 1003 | 05:31 |
| 9. The cautionary tale of James Raventos | 1 | 310 | 01:28 |
| 10. Simulating fear in patients | 259 | 04:14 |

We, first of all, took our drugs into... human beings at St George's Hospital in London, now a big Lanesborough Hotel, and the first subject that we used it on was a young doctor. And, if you infuse isoprenaline into an artery in the arm, the... the blood flow... the blood vessels in this whole arm would dilate, and you could measure the big increase in blood flow which isoprenaline would produce, so you measure it and then you infuse the drug, just locally, and then you put the isoprenaline in again and be completely blocked in. And then we, almost without pausing for breath, then went to another young doctor and he is now given isoprenaline intravenously, so the whole body gets it, and on the control you... not only does his heart rate go whipping up and he gets a fall in blood pressure and an increase in blood flow to... to his arms, but he... he's restless. And afterwards I... I... you know, 'What's the problem?' He says, 'I feel I'm going to die'. And, so then we treated him with pronethalol and now – isoprenaline was given again – all is peace. Heart rate doesn't change, blood pressure doesn't fall, blood vessels don't dilate, and he's lying at peace. So, this... so, this was where, you know, one got the idea that one's heart is sending information into the brain all the time and relating, if you like, the appropriateness of what it's doing to what the whole body's doing, so if, in this case, the guy is lying on the bed and you stimulate the heart fast enough, as though he was running from a lion, but there's no lion, all hell goes loose upstairs, something's gone wrong here, and so they get this fear. And, this has always been one of the things which have in... been involved with beta blockers... is this business about using them to control fear for examinations, billiard players, musicians. I have a friend who's a concert pianist and when he... in the old days you would come on for the first part and you'd feel passionate, and then go off at the interval, your shirt was soaked, change it, shower, and you've come back on for the second half, and now you're washed out and you're passionless. And what beta blockers did was allow them to be much more intellectual, so the first half they could play but didn't get too worked up about it, and then... so they got a more uniform performance. Whether that was good or bad he wasn't sure, but that's what they did. So, that was the first thing. Then we... we moved to University College to a chap called Brian Prichard – a young clinical pharmacologist – and he found that when he took his patients and gave them pronethalol that the pulse rate would fall, but he found that only a few of the patients with the initial dose he... would the blood pressure... would the pulse rate fall. But he found if increased the dose more and then... so he was able to show that eventually, if you give a big enough dose, he could get the pulse rate down to 60 at rest in everybody.
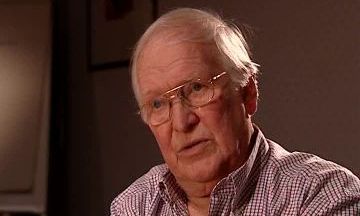
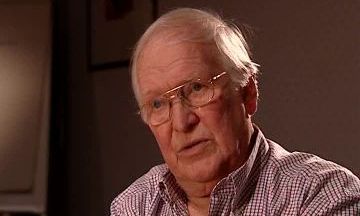
The late Scottish pharmacologist Sir James W Black (1924-2010) revolutionised medical treatment of hypertension and angina with his invention of propranolol, the first ever beta blocker. This and his synthesis of cimetidine, used for the treatment of peptic ulcers, earned him the Nobel Prize in Physiology or Medicine in 1988.
Title: Simulating fear in patients
Listeners: William Duncan
After graduating with a BSc Bill Duncan went on to gain a PhD from Edinburgh University in 1956. He joined the Pharmaceuticals Division of ICI where he contributed to the development of a number of drugs. In 1958, he started a collaboration with Jim Black working on beta blockers and left ICI with him in 1963 to join the Research Institute of Smith Kline & French as Head of Biochemistry. He collaborated closely with Black on the H2 antagonist programme and this work continued when, in 1968, Duncan was appointed the Director of the Research Institute. In 1979, he moved back to ICI as Deputy Chairman (Technical), a post he occupied until 1986 when he became Chairman and CEO of Coopers Animal Health. He ‘retired’ in 1989 but his retirement was short-lived and he held a number of directorships in venture capital backed companies. One of his part-time activities was membership of the Bioscience Advisory Board of Johnson and Johnson who asked him to become Chairman of the Pharmaceutical Research Institute of Johnson and Johnson in New Jersey. For personal reasons he returned to the UK in 1999, but was retained by Johnson and Johnson until 2006 in a number of senior position in R&D working from the UK. From 1999 to 2007 he was a non-executive director of the James Black Foundation. He is now fully retired.
Tags: St George's Hospital, The Lanesborough Hotel, UCL, Brian Prichard
Duration: 4 minutes, 14 seconds
Date story recorded: August 2006
Date story went live: 02 June 2008