So that took us really up to the late '60s, at which time, one could say with some certainty, what was not wrong with thalassemia, but we still don’t, didn’t know what was wrong. You could, either there was going to be, for some reason, a decreased amount of normal message, or there was going to be some subtle molecular abnormality that none of us understood. And then we of course moved into the Nuffield, and into the, into the, the Institute of Medical Genetics in Liverpool, which you came about '69 I guess, yeah, that’s right. And there were two interesting, I think those early years when you were in the lab, that’s between about '60 and '65, were really exciting years actually, because we were able to diversify our interest a bit, obviously. Like everybody else in the field, we were interested in foetal haemoglobin, and looking for natural models, like the ones that you looked at in pregnancy and so on, and we were still looking for natural models which might lead us into the thalassemia molecular field, and something came along, I think it was about 1971, it just was a letter from Jamaica, from a chap called Paul Milner who said he’d got this family with alpha thalassemia, with haemoglobin H disease. And he’d, he’s had a funny electrophoresis, because there was some tiny amounts of a funny haemoglobin, which he’d not seen before, and I was just looking at the correspondence the other day, and I wrote back and said, well, could this be a very badly synthesised alpha chain, let’s have a look. And, that was, again, by this time, Clegg and I, we really did work extremely well together, but we knew how to split the work, because Clegg hated blood, or anything red, it made him sick, so I used to do all the kind of initial preparations and then give the purified white powder to Clegg, and making purified amounts of this tiny amount of material, it’s about 1% of the total haemoglobin, but we used to do a lot on amberlite exchange columns those days, and if you fixed the molarity of the phosphate buffers adequately, you could separate a lot of different haemoglobins, and we knew that with conditions where things like A2 and that would stick tight, and you could wash off everything else, so prepared an enormous amberlite column, you know, kind of pornographic thing, and shoved grams of this haemoglobin from one of these patients on top of this column, and just went washing it day after day until it was clean of everything that would come off it, and then just poured some concentrated salt across the top, and this band came down, and so I was able to present Clegg, I think in end with about three or four milligrams of semi-pure haemoglobin which we later called haemoglobin Constant Spring, because the family came from Constant Spring, which was a little suburb of Jamaica- of Kingston. Anyway, Clegg was very surprised when he fingerprinted this to see that, you know, a few extra peptides which weren’t there normally. And when he strung them together it was clear that this was an extended alpha chain of about 30 residues, and if you looked at the structure, what clearly had happened was that the normal termination code, which is UAA normally, had changed to CAA or something like that, and had put glutamine in instead of terminate.
[unclear]
Yeah, and this suggested that there was message beyond the normal termination code, and which was not normally used till you reach another in phase stop codon on, and actually, you could even, from the amino acid structure, anticipate what the, what the nucleotide sequence would be. So we, we published this stuff in, in Nature, and the, our friends in Cambridge at Fred Sanger’s lab were all working on the structure of human message, Nick Proudfoot and Tito Baralle, and they told you, you know, bloody amateurs that there’s a load of old rubbish here. It was really great actually, because when they got alpha globin message sequences exactly what I predicted from Constant Spring. So that was one molecular defect, a chain termination mutant with the production of a tiny amount of mutant haemoglobin.
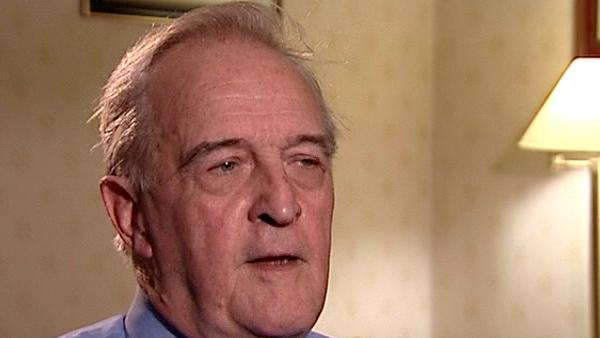
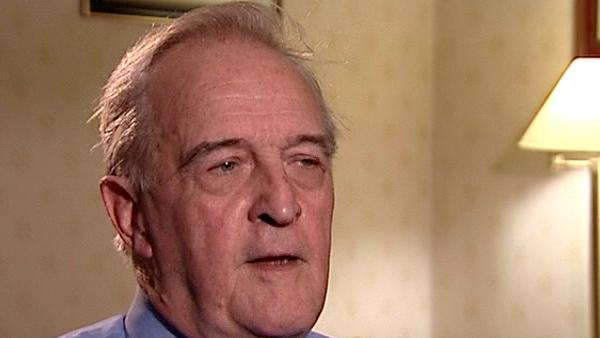
British Scientist Sir David Weatherall (1933-2018) was a world renowned expert on blood diseases, in particular thalassaemias, and used his expertise to help control and prevent these diseases in developing countries. He founded the Institute of Molecular Medicine at Oxford in 1989 and was knighted in 1987.
Title: A family with alpha thalassemia in Jamaica
Listeners:
Marcus Pembrey
Marcus Pembrey, now Emeritus, was Professor of Paediatric Genetics at the Institute of Child Health, University College London and consultant clinical geneticist at Great Ormond Street Hospital for Children London. He is a visiting Professor at the University of Bristol UK, where he was the Director of Genetics within the Avon Longitudinal Study of Parents and Children until 2006. A past president of the European Society of Human Genetics, he is also the founding Chairman of the Progress Educational Trust.
Duration:
5 minutes, 9 seconds
Date story recorded:
July 2007
Date story went live:
02 June 2008