We started off in the Department of Medicine with very little space, but my predecessor, Paul Beeson had got me there a little bit early, so that I could help in planning the John Radcliffe hospital, the new hospital in Oxford, and the Department of Medicine had a little bit of space and by then we’d kind of recruited, we had Doug Higgs developing his alpha chain interests, and we were starting just in that period before we moved to Oxford, with the preliminary kind of sorties into prenatal diagnosis. People had tried to use that chain method for globin chain analysis that we developed, and, because Bill Wood, when he was doing his thesis had shown that there were very small amounts of normal beta chain made very early during development, in some ways it makes you think about intelligent design almost, I mean, why on earth do we make, start making our adult haemoglobin that early, you know, right back at 15 weeks, 14 weeks, even earlier? And so it was becoming clear that if you could do globin synthesis on some form of foetal blood, there might be a chance, and I must say, our group, we were always more cautious than other people I think, and we were very nervous that that method would never be sensitive enough, but Kan, in the States and Modell here, just came and banged on our door, and said do it, and teach us how to do it, so we did, and both sides of the Atlantic, it started to work. And that was all just happening in that changeover period. It was, I, I think actually, looking back on that, it was I suppose quite gratifying at the time, because the methods for obtaining foetal blood, I mean, at first they were just prodding the placenta, and then having to try to purify the foetal cells and then, but then when the actual foetal blood sampling became, from the cord, became possible, that technology worked, and it worked for about ten years really, and was applied very widely in the Mediterranean, and here of course and in the States, and the foetal loss rate was gradually came down, the error rate came down, so it was quite a gratifying period, and of course it was taken over by DNA analysis. So that was the period of kind of interregnum before moving up to the John Radcliffe labs, and we had more space there, we started to recruit one or two more people and Kay Davis came and joined us for a while then, and we had an extraordinary character called Steve Reeders, who was a nephrologist who joined us. Just plonked himself down in my office, and said- I’m going to find the gene for polycystic kidney disease, so I said- oh, yeah, good luck, and of course we had this strong alpha chain group. I was particularly interested at that time in trying to expand our work, we were already kind of interested in malaria from the population genetics point of view, but more actually into the, into the kind of cellular mechanisms involved in all that, and so we were starting to diversify basically, and so during that period, I suppose the most interesting work was the beginning analysis of the alpha and beta thalassemias by Southern Blotting, and Doug Higgs got into that very early and it was very competitive with the Americans and in fact, over the next few years I think, it was really our group that characterised most of those important common deletions in, of both alpha zero and alpha plus thalassemia. As regards the malaria programme, I’d started that down in the John Radcliffe with a post-doc Rhodes scholar actually, Geof Pasvol, and again, we followed technology, because it just, in the kind of early 70s became possible to grow malarial parasites in culture. Ridiculous, people had tried for years, and then the group at Rockerfeller just found by accident that if shoved some of them in a bowl at reduced oxygen tension, they grew fine. And so we could, you could start to do in-vitro invasion studies at that stage, and we found that poor old Haldane was probably wrong actually, the, because he’s suggested that those little red cells the parasites wouldn’t, couldn’t get in, or if they got in they got kind of squashed, but they seemed to grow and develop beautifully in thalassemic cells. But the sickle cell story was quite interesting, in that if you did the incubations at oxygen tensions were, you would fine in the kind of venous cell to the circulation, the parasites didn’t develop and there were similar conclusions by the New York group, and also by Luzzatto, with a, using another method, and the idea of kind of suicidal infection and a parasite gets in a sickle cell and can’t complete its life cycle. It’s not bad, you never absolutely prove that, but it’s not a bad mechanism.
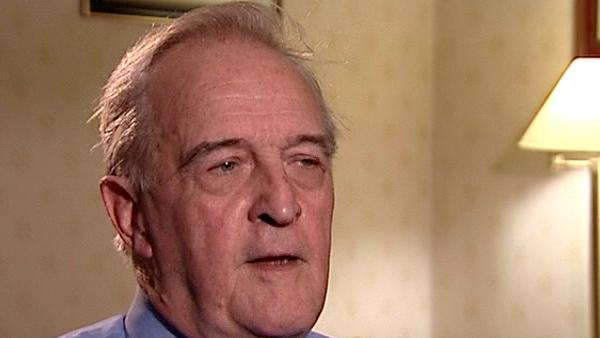
British Scientist Sir David Weatherall (1933-2018) was a world renowned expert on blood diseases, in particular thalassaemias, and used his expertise to help control and prevent these diseases in developing countries. He founded the Institute of Molecular Medicine at Oxford in 1989 and was knighted in 1987.
Title: Work at the Department of Medicine at Oxford
Listeners:
Marcus Pembrey
Marcus Pembrey, now Emeritus, was Professor of Paediatric Genetics at the Institute of Child Health, University College London and consultant clinical geneticist at Great Ormond Street Hospital for Children London. He is a visiting Professor at the University of Bristol UK, where he was the Director of Genetics within the Avon Longitudinal Study of Parents and Children until 2006. A past president of the European Society of Human Genetics, he is also the founding Chairman of the Progress Educational Trust.
Duration:
6 minutes, 18 seconds
Date story recorded:
July 2007
Date story went live:
02 June 2008